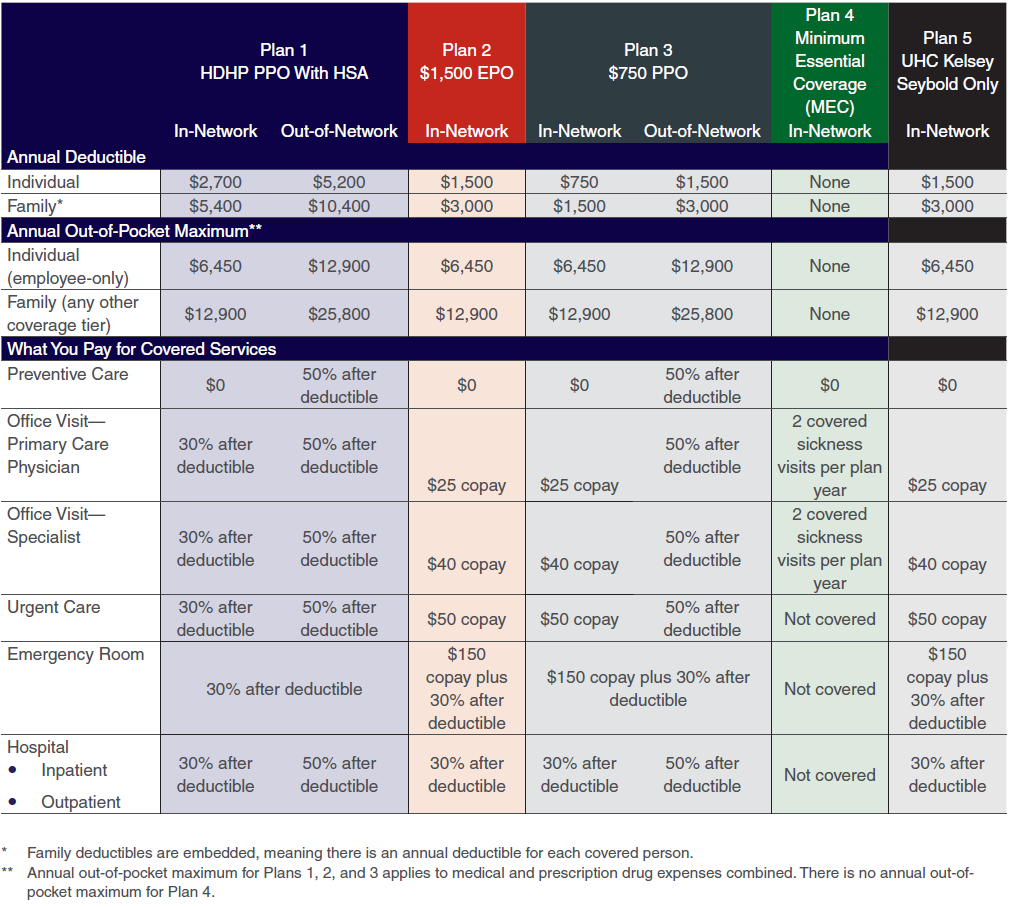
Brock offers three health plans options through BlueCross BlueShield of Texas. The Minimum Essential Coverage (MEC) and Kelsey-Seybold Only plans are offered through UnitedHealthcare (UHC).
You pay low monthly premiums, the highest annual deductible, and have the opportunity to contribute to a Health Savings Account (HSA).
You pay higher monthly premiums and a lower annual deductible, and can only access medical care in-network.
You pay higher monthly premiums and a lower annual deductible, and can only access medical care in-network.
Additional Information
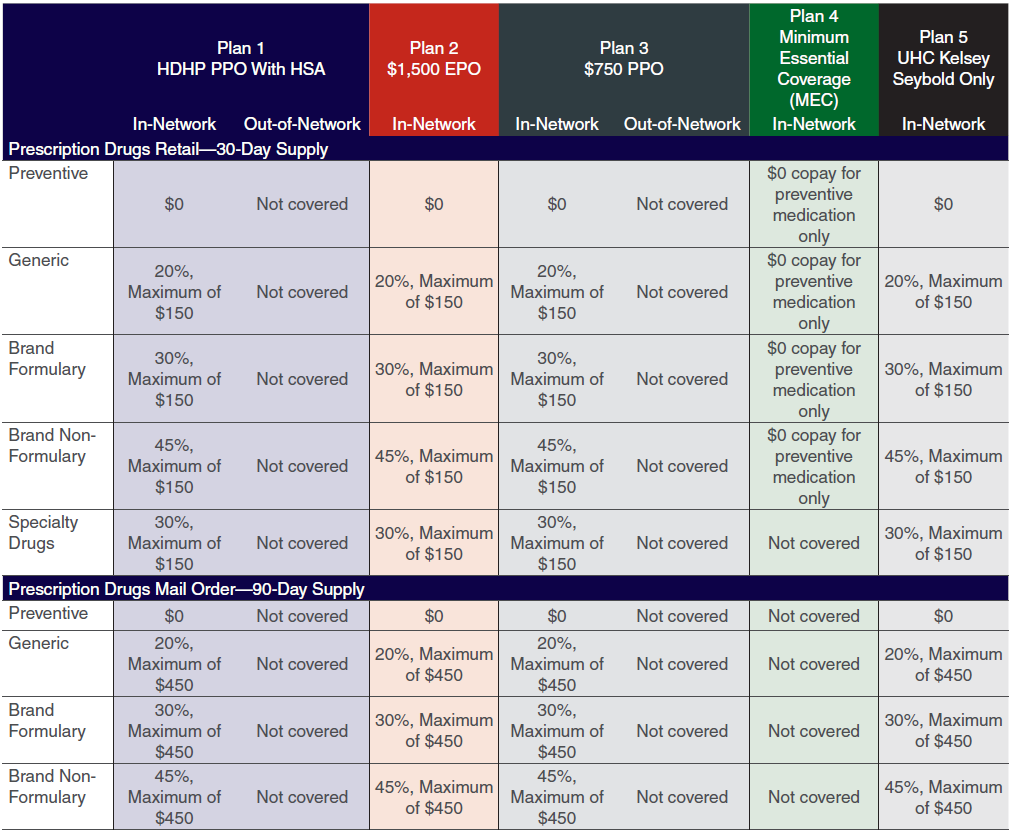
Your medical coverage includes prescription drug benefits through BlueCross BlueShield of Texas or through UHC if enrolled in the Minimum Essential Coverage (MEC) plan. It’s important you understand the different types of prescription drugs, as the type of drug you get can have a big impact on your out-of-pocket costs.
- Preventive — Drugs that keep you from developing a health condition. Your plan provides a list of medications to support your goal of ongoing good health and helping to reduce your overall health care costs.
- Generic — A more cost-effective alternative to brand name drugs with the same active ingredients.
- Brand Formulary — Brand-name drugs that may have no generic equivalent.
- Brand Non-Formulary — More expensive brand-name drugs that do have an alternative generic equivalent.
- Specialty Drugs — Drugs that include high-cost injectable, infused, oral or inhaled drugs that generally require special storage and handling and close monitoring of the patient’s drug therapy.
Before you enroll, call Health Advocate at 866.799.2691 to confirm in-network and out-of-network coverage in our plan.
After enrollment, new ID cards will be issued to all employees who elect a BCBSTX medical plan. Your health plan or network will be shown on the front of your ID card. If you have questions about which network you have, call the Customer Service number on the back of your card. To see the most accurate list of providers, register or log in to Blue Access for Members at www.bcbstx.com.
Note: Brock advises all employees and/or dependents to seek personal, individual advice based on individual facts and circumstances from an independent tax advisor regarding the tax consequences of specific health benefit plans, products or services, including the HDHP.